North Carolina will offer enhanced Medicaid reimbursements to hospitals that forgive medical debt and adopt policies designed to prevent further debt from accruing, North Carolina Gov. Roy Cooper said in a press release Monday.
North Carolina is one of at least 17 states, cities and counties that have passed policies attempting to erase debt or block future medical debt from increasing, according to a recent analysis from center-left think tank the Third Way.
However, the Tar Heel State is the first to tie additional Medicaid dollars to reducing medical debt and enhanced charity care. The carrot approach represents a “major new way of doing [things],” according to David Kendall, senior fellow for health and fiscal policy at the Third Way.
To participate, hospitals must erase current Medicaid enrollees’ medical debt deemed uncollectible going back to Jan. 1, 2014 and non-enrollees’ debt who who earn below 350% of the federal poverty level, or whose debt exceeds 5% of their annual income.
Hospitals must also enhance their charity care policies by providing discounts on care for patients who make below 300% of the federal poverty level, automatically enrolling patients in financial assistance programs, and agreeing not to sell medical debt to debt collectors or report debt covered by these policies to credit reporting agencies.
The program has the potential to erase up to $4 billion in existing medical debt across the state, according to Cooper.
The governor received approval from the CMS for the plan on Friday, according to the release.
The initiative comes as North Carolinians are struggling with rising medical costs, and pressure is rising on the state’s nonprofit health systems to overhaul their charity care policies.
A recent KFF analysis found the state ranks among the highest in the nation for medical debt, with 13.4% of adults reporting they carry medical debt.
Meanwhile, a joint investigation from Duke Law School faculty and the Office of State Treasurer published last year found that North Carolina hospitals sued over 7,500 patients and their family members between January 2017 and June 2022 to collect medical debt. The lawsuits often followed patients not being offered sufficient charity care, according to interviews with patients.
In the wake of the investigation, Charlotte-based Atrium Health, a major healthcare provider in the region, ended its policy of suing patients with unpaid bills in 2023. The system had been behind 2,482 of the lawsuits filed between 2017 and 2022.
North Carolina’s program was described by multiple analysts as a “win-win” for patients and providers.
While multiple other localities have used a carrot-based approach to entice hospitals to adopt better charity care policies, they have typically leveraged one-time funds to buy existing debt, according to Kendall. For example, Cleveland allocated American Rescue Plan Act dollars to buy medical debt following COVID-19.
Under North Carolina’s model, hospitals will receive more funds to serve low-income patients.
“Using ... enhanced Medicaid payments as an incentive is a good strategy that would seem to have ... a chance of permanently changing behavior as compared to a one-time injection of funding,” said Katherine Hempstead, senior policy advisor for the Robert Wood Johnson Foundation. “The likelihood of states opting into the program... [is] pretty high, unless the incentives are very low because otherwise hospitals that don’t opt in will lose ground competitively to those that do.”
She added that “a lot of medical debt is not collectible anyway, so the cost to participate may not be that great.”
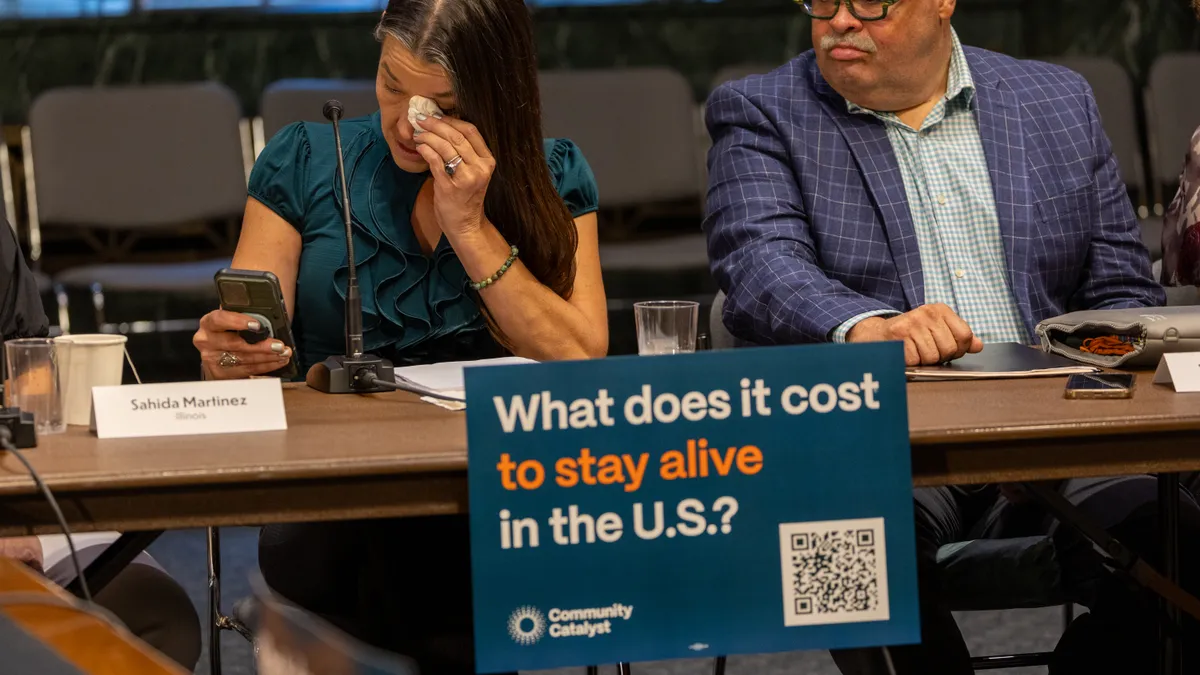
Mona Shah, senior director of policy and strategy at Community Catalyst, a health justice advocacy organization, called North Carolina’s approach “groundbreaking” and hoped other states would follow suit.
Still, despite analysts’ enthusiasm, it isn’t immediately clear whether health systems will sign onto Cooper’s plan.
Healthcare Dive reached out to the state’s largest health systems, as well as the health systems named as the top offenders in last year’s OST report, including Atrium, CaroMont Health, Community Health Systems and Sampson Regional Medical Center.
Health systems either didn’t respond to requests for comment or said they didn’t yet have enough information about the incentive program to determine whether they would participate.
A spokesperson for Novant Health said they “look forward to receiving finalized operational details from the North Carolina Department of Health and Human Services so that we can ensure the program requirements do not conflict with separate legal obligations or fall short of our industry-leading financial assistance policies.”
UNC Health likewise said it supports “efforts to reduce medical debt,” however, it will need to “take time to understand the potential impact and to implement the policy.”